Written by Marv Law
We often receive calls from people having issues with their Medicare coverage and asking what they can do about it. Sometimes simply understanding their coverage helps them to resolve their issue. However, other times it may require them to change plans.
Although options are limited during the year outside the Annual Enrollment Period from October 15 to December 7, there are some Special Enrollment rules that may allow people to change their plan.
Recently Moved. People who change their permanent residence often have new options in their new zip code and may be eligible to change plans.
Loss of Coverage. When someone is no longer eligible for an employer plan because of retirement, or must leave a spouse’s plan because of divorce.
Special Needs. People with chronic illnesses such as diabetes or heart disease sometimes qualify for a Special Needs plan and might be eligible to change plans one time.
Birth Month. For those on a Medicare Supplement (different than a Medicare Advantage Plan) there is an opportunity to review and change plans that might be more cost-effective.
Five Star Plan. If a Medicare Advantage Plan attains a Five Star rating from Medicare, members are allowed a single special enrollment period during the year.
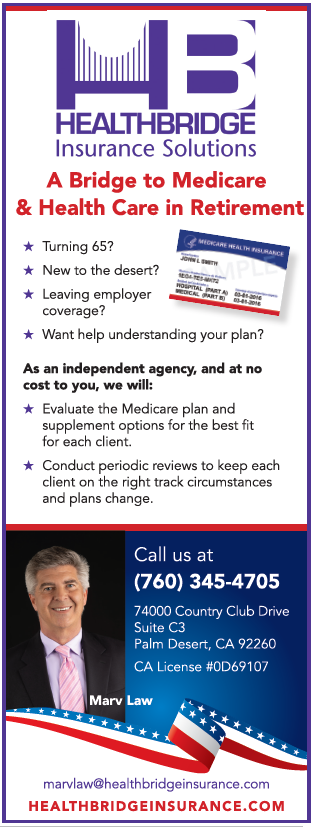
An experienced and knowledgeable local independent agent who contracts with many highly rated companies and plans can help you understand your plan, or navigate the maze of options for the best fit for you at the right time. Give us a call at 760-345-4705 or email Marv at [email protected]